How Does Thermography Work?
Modern Thermologists use digital cameras that record infrared radiation emitted by the human body and convert them into temperature readings and plot them on a computer screen. Thermologist’s are then able to identify areas of hot and cold in relation to the opposite side of the body. Areas with decreased blood flow will have colder temperature readings and areas of increased blood flow will have warmer temperature readings.
Breast tumors and some other tumors are able to found on thermal imaging through the process known as Angioneogenesis, the formation of new blood vessel that supply nutrients to a tumor. This asymmetric increase in blood flow creates an increase in temperature that can be picked up by medical thermal cameras. Many times this blood supply increases over time as a tumor grows and is an important part of baseline studies and the ability for them to identify a tumor at the earliest possible moment.
Thermography History
Breast Thermography was introduced in Quebec Canada in 1956 by Dr Robert Lawson who published the first medical paper on breast thermography on 26 women with breast cancer. His research showed that women with breast cancer had over a 2 degrees delta T when comparing the pathological breast with the opposite side. In the 1960’s infrared cameras were introduced and the first Barnes Thermograph was patented. Later liquid crystal bras and plates were used as a more affordable method of screening.
In 1972, the Department of Health, Education and Welfare declared that Breast Thermography was ‘Beyond Experimental.’ Over 4000 articles were published on thermography and over 800 focused on breast thermography. All major medical institutions implemented the technology in the USA. Other countries adopted the use as well.
The above image is that of the first thermal study performed by Robert Lawson in Quebec, CA in 1956. This was published and can be found in PUBMED
Thermography vs Mammography
Thermography is a reliable and comfortable adjunctive procedure that is used in conjunction with traditional screening methods for conditions including breast cancer. Please understand that Thermography is NOT a stand-alone diagnostic test, but it provides valuable additional information that can be used in a holistic screening approach.
Indeed, there have been instances where thermography has helped identify areas of concern in women who have undergone mammography with no detected issues. The November 2012 issue of the New England Journal of Medicine discusses the potential benefits of integrating different methods for a comprehensive screening strategy.
Thermography has additional importance in addressing the often overlooked demographic of women under the age of 40, and those with dense breasts. These groups sometimes present challenges for traditional screening methods. Annually, over 20,000 cases of breast cancer occur in the US in the under 40 age group, and the nature of the disease in these cases tends to be more aggressive, less responsive to treatment. Currently, there’s no routine screening protocol for these women.
In this context, thermography offers potential as a useful adjunctive screening procedure. It does not replace any existing methods, but can be an important tool in the arsenal of preventative healthcare for women of all ages and conditions. This potential of thermography warrants further investigation and research to continue enhancing women’s health practices.
Breast Thermography Exam Process
Thermography is a non-invasive physical test that takes approximately 15 minutes. This process doesn’t exert any pressure on the breast, differentiating it from some other screening tests. It leverages digital infrared imaging to identify any symmetrical variations in the breast. Women with implants or those who have undergone a mastectomy may require specialized evaluation procedures, but can still benefit from this test.
The thermography test is conducted in the healthcare provider’s office. Initially, the patient will be asked to complete a breast history form. The examination takes place in a private setting, often separated by a curtain for patient comfort and privacy. To align the patient’s body with the room’s temperature, a settling period of 10-15 minutes is necessary before imaging.
The patient is then positioned in front of the thermography system to capture images of the upper chest, underarms, and breasts. The infrared imaging camera takes these images and stores them for future comparisons, establishing a baseline over time. This technology can provide clear insights into vascular patterns, temperature variations, and potential physiological conditions.
Once captured, these images are interpreted by a PACT (Professional Academy of Clinical Thermology) Certified Clinical Thermologist. They will process and grade the images digitally, adhering to the standardized reading protocol set by PACT. This methodical process ensures the utmost reliability and consistency in screening
Importance of Breast Thermography Follow-up
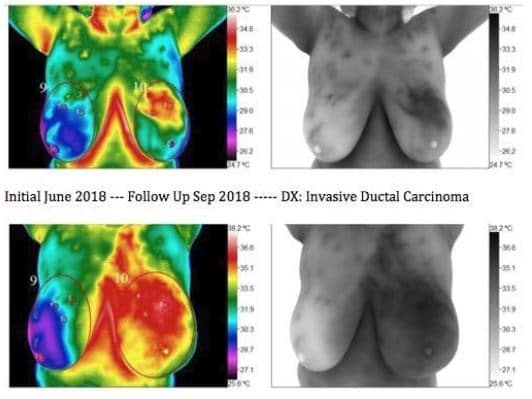
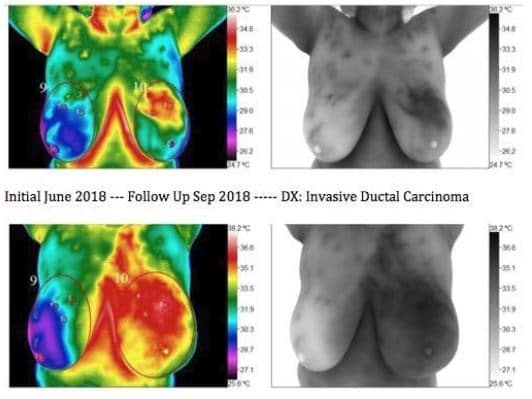
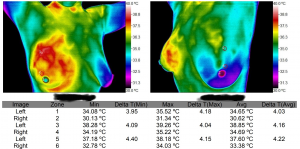
The images were taken at 3-month interval. As it is seen here the progression of Breast Cancer can be rapid. Proper follow-up ask directed by the interpreting thermologist can not be over-stressed, as the caveat in thermography is the perceived non-importance, or trying to compare it to mammography.
Overall Breast Health and Thermography
We are at the cutting edge in technology and have seen some remarkable presentations in the physiology of the body. We are pioneering areas that have never been seen before. One of these areas is in the area of toxicity. We have established a relationship between Hormone Toxicity/ Fibrocystic Breasts and small pockets of inflammation that we describe as “leopard spots”.
More properly these areas are sequestered areas of inflammation due to toxins(irritants) in the form of several possibilities. Through massive deduction of hundreds of thousands of cases we theorize these points are aberrant and only found in pathological patients. We have established this through clinical experience and intense study of specific habits of our large patient base. For example, we notice an absence or minimization of these spots in patients who live a toxin free life and adhere to strict diet and lifestyle.
We need a large study of this nature but understanding that studies of this size only are performed for drug companies we will probably never see one. The best we can offer at this point is our experience and observations until we can fund such a study.
Why Opt for Breast Thermography?
Breast Thermography, cleared by the FDA, provides a supportive role in the detection of breast cancer, enhancing your overall health strategy. What makes Breast Thermography an attractive choice?
- It prioritizes your safety: Thermography is a 100% safe method to use.
- Offers a radiation-free approach: No radiation is involved in the process, giving you peace of mind.
- Maintains your comfort: The process is contact-free and compression-free, ensuring a comfortable experience.
- Convenience is key: The procedure is straightforward, making it a convenient addition to your health routine.
- Inclusive of All Women: Thermography is a versatile tool that can be utilized irrespective of breast density or the presence of implants, making it an accessible option for all women.
- Helps establish a personalized health baseline: With thermography, an individualized baseline of your breast health can be established.
- Available to younger women: It serves as an effective supplemental tool for women under 40, who often aren’t included in current breast cancer screening guidelines.
- Based on extensive research: With over 30 years of research and 800 peer-reviewed articles, the technique is backed by extensive scientific evidence.
Factors Affecting the Results of Breast Thermography
Not all tests are perfect or 100 percent accurate. It is important to combine testing for optimal outcome. The following will limit successful outcome measurements to a point”
- Patient’s age
- Ability to stay still in the proper positions
- Excessive use of bras
- Seat warmers, over exercising, caffeine use
- Medications usages including hormone pills and birth control
- Obesity
- Extra large breasts
- Implants
The Promise of Breast Thermography
Thermology has become a valued and recognized tool in the scientific community. It is used in many disciplines of science and is growing as a viable choice for imaging the physiology of the human body. Thermography should be used by medical personnel in the fight against breast cancer and the promotion of breast health.
 Breast Thermography is a non-invasive and painless way to screen for breast cancer without radiation or compression of the breast. It uses state of the art medical infrared technology to assess heat in the breast. Comparative exams create a baseline for monitoring breast health based on individual thermal patterns and changes.
Breast Thermography is a non-invasive and painless way to screen for breast cancer without radiation or compression of the breast. It uses state of the art medical infrared technology to assess heat in the breast. Comparative exams create a baseline for monitoring breast health based on individual thermal patterns and changes.