- Home
- Breast Thermography
Breast Thermography
Safe, Insightful & Non-Invasive Screening
Enhancing Breast Health with Advanced Thermography
At Breast Thermography International (BTI), we have over 30 years of experience providing high-quality, FDA-cleared breast thermography services.Our approach to breast health emphasizes awareness, ongoing monitoring, and patient comfort, all without additional radiation or compression.
Thermography offers valuable physiological insights, making it an important part of a comprehensive breast health strategy.
Understanding Thermal Imaging for the Breast
What is Breast Thermography?
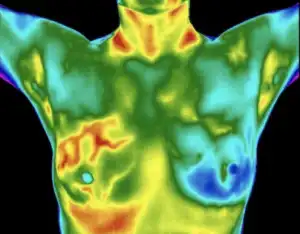
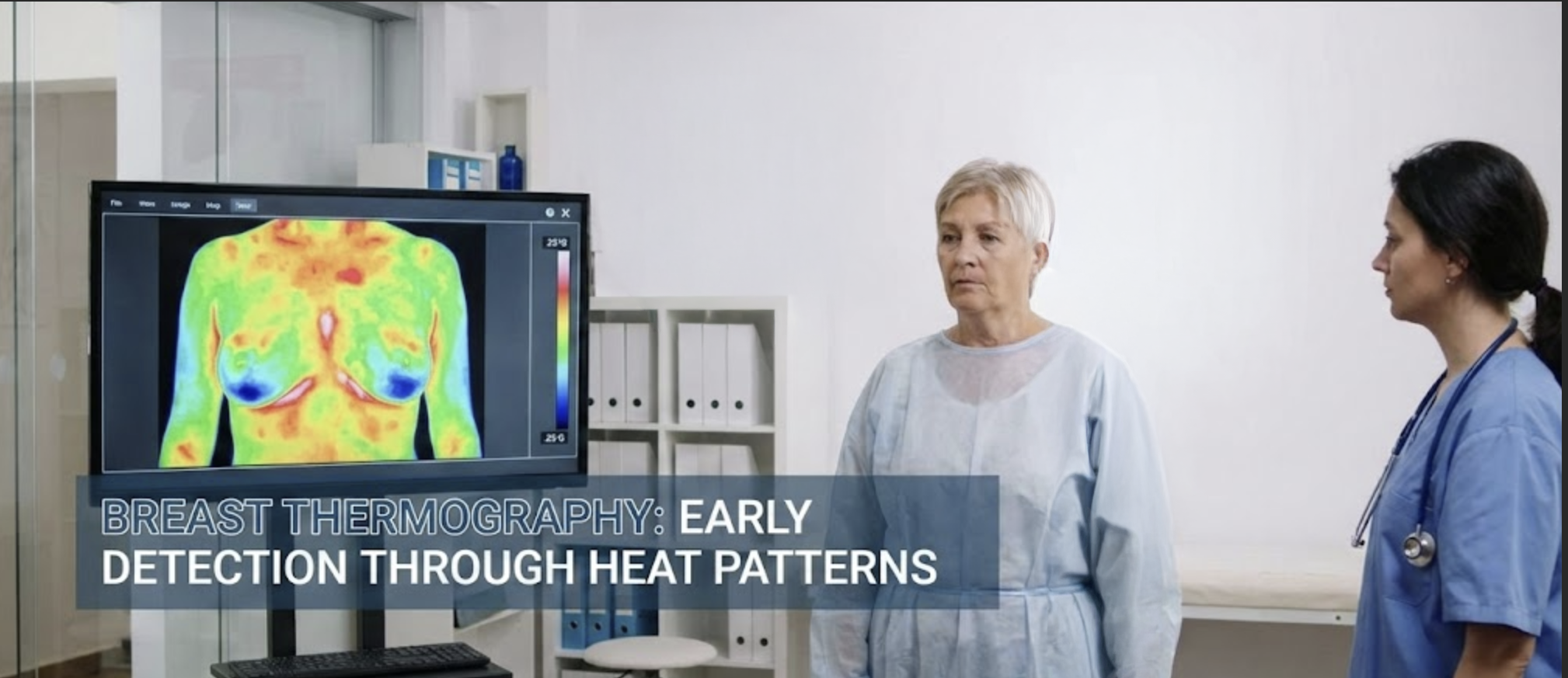
Breast thermography, also known as digital infrared thermal imaging (DITI), is a non-invasive technique that captures and analyzes heat patterns and blood flow in breast tissue. By detecting subtle temperature variations, thermography provides insight into physiological activity that other imaging methods may not reveal.
Unlike structural imaging, thermography does not require ionizing radiation, making it a safe and repeatable option for regular breast health monitoring. This can be especially useful for those with dense breast tissue or individuals seeking a radiation-free imaging method as part of a broader screening plan.
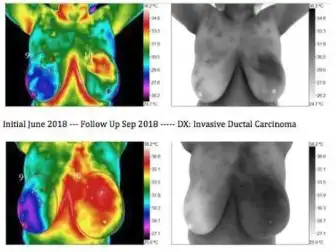
Research has shown that thermal imaging can detect abnormalities related to blood vessel growth and inflammation. While thermography does not diagnose conditions, it serves as a useful adjunctive tool for monitoring physiological changes over time.
Enhancing Traditional Screening Methods
A Complementary Tool for Breast Health Monitoring
Breast thermography is an adjunctive tool that can be used alongside other imaging methods, including ultrasound, MRI, and mammography. Each of these techniques provides different information, and thermography focuses on detecting functional changes such as increased blood flow or metabolic activity. When integrated into a breast health strategy, thermography offers an additional perspective that can help track changes over time.

Benefits of Thermography at a Glance
Why Consider Breast Thermography?
- Detects abnormal heat patterns in breast and abdomen.
- Indicates possible lymphatic system involvement.
- Tracks spread of cancer through thermal imaging.
- Highlights inflammation linked to cancer cells.
- Supports diagnosis and staging of breast cancer.
- Identifies potential for metastasis early.
- Visualizes cancer progression in real time.
- Non-invasive tool for monitoring cancer changes.
How the Thermal Scan Is Performed
How Breast Thermography Works
A high-resolution infrared camera captures thermal images of the breast tissue, which are then analyzed for patterns related to blood vessel activity, temperature asymmetry, and other physiological markers.
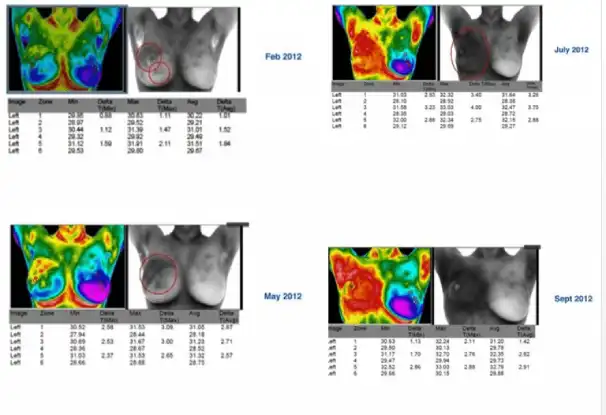
Since thermography monitors functional activity, it is most effective when used as part of an ongoing health strategy. A baseline scan is typically performed first, followed by comparative scans over time to track any significant changes.
Patients undergoing thermography should avoid certain activities before the scan, such as exercise, caffeine, or using lotions on the skin, as these can affect the thermal imaging results. Proper preparation ensures a more accurate scan.


Expertise You Can Rely On
BTI: A Trusted Leader in Breast Thermography
With over three decades of clinical experience, BTI has been at the forefront of breast thermography research, training, and application. Our certified professionals follow rigorous standards to ensure each thermographic assessment is performed with expertise and precision.
We are committed to providing advanced technology and reliable results. Every scan is conducted in a professional setting using FDA-cleared infrared imaging systems, ensuring high-quality imaging and thorough analysis.
Empower Your Breast Health Journey
Taking a Proactive Approach to Breast Health
Breast thermography is an excellent option for individuals looking to take a proactive approach to their breast health. Used as a monitoring tool in conjunction with other imaging methods, thermography offers a unique perspective on breast physiology.
By integrating thermography into a comprehensive breast health plan, individuals can gain a broader understanding of their breast health, allowing for more informed decisions.